Photosensitive Epilepsy: How Light Can Trigger Seizures
Key Highlights
- Photosensitive epilepsy is characterized by having certain light and/or patterns trigger seizures and related symptoms
- Photosensitive epilepsy more commonly occurs in children and young persons, and it may disproportionately affect women
- A variety of light sources, features and patterns can aggravate photosensitivity, namely flashing or strobing lights, high-contrast sources, and exposure to specific wavelengths
- Managing photosensitive epilepsy is possible with behavioral and lifestyle modifications, such as activating safety features for online use and wearing specialty photosensitivity glasses
Epilepsy affects around 50 million people worldwide, making it one of the most common neurological conditions, according to the World Health Organization. For a small portion of those individuals—about 3 to 5 percent—light can actually trigger seizures and other symptoms. This form of epilepsy is known as photosensitive epilepsy. In this post, we’ll take a closer look at what it is, how light plays a role, and what people living with it might need to be aware of in everyday life.
What is Photosensitive Epilepsy?
Photosensitive epilepsy is a condition whereby symptoms can result from exposure to certain visual stimuli, predominantly related to light. The development of epilepsy can stem from a specific cause such as head or brain trauma as well as a stroke, but the majority—including photosensitivity—is believed to have a genetic link.
Photosensitivity is more common with specific types of epilepsy, specifically juvenile myoclonic epilepsy, and may affect 40% of patients with this particular condition. It also seems to disproportionately affect more women than men; the onset of the condition also tends to occur during early adolescence.
This may be further exacerbated by children and teens’ increased exposure to potential triggers such as cartoons, electronics, and video games. A person also does not need to be specifically diagnosed with photosensitivity in order to have a light-provoked seizure; researchers have suggested that any person with epilepsy may have as high as a 14% chance of experiencing a seizure brought on by light exposure. Even people without epilepsy can be susceptible, particularly younger persons, with recent analyses showing that some can experience the same brain responses to intense or flashing lights.
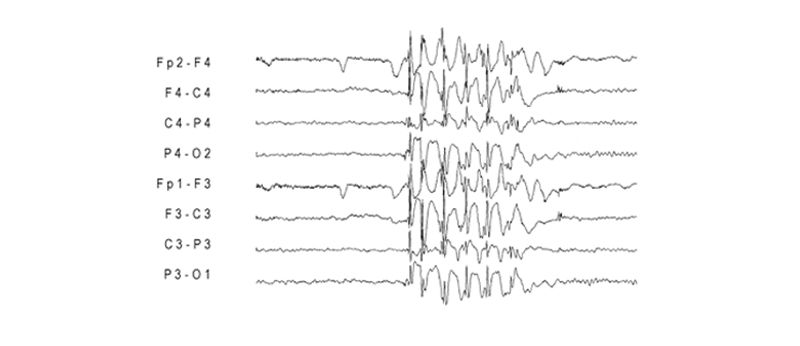
Recorded brain activity from a photosensitive epilepsy patient. Source: PubMed.
Photosensitive Epilepsy and Comorbid Headache Disorders
Headaches—especially migraine-like ones—are surprisingly common in people with photosensitive epilepsy. In fact, individuals with epilepsy are more than twice as likely to experience migraines compared to those without the condition, and photosensitive patients often report headaches triggered by the same flashing light exposure that provokes seizures.
Researchers believe that altered brain excitability may underlie both conditions, and migraine with aura symptoms often mirror the experiences of a photosensitive seizure—making them more connected than they may first appear.
Types of Light That Triggers Seizures
For those with the condition, various types of light sources may stimulate the eye and brain in extreme ways. These triggers result in seizures due to irregularities within the brain or unbalanced neurotransmitters (chemical messengers). And it doesn’t take long either: exposure for as little as 4 minutes can cause a seizure! The Epilepsy Foundation cites the following common light-related triggers:
Speed or flicker (including fluorescent lighting)
Flashing or "high frequency" light sources are often triggering for those with photosensitive epilepsy. Frequencies of about 5-30 flashes per second are more likely to induce a light-triggered seizure. Common triggers might include television programs, cartoons, movies, video games, and concerts.
Fluorescent lighting poses its own special risk. Studies have shown that faulty fluorescent lights which produce a visible flicker can trigger epileptic brain activity. In addition, although researchers remain mixed, fluorescents as well as certain LED, television and computer screens can create an invisible flicker that is picked up the brain and could lead to seizures or elevated neurological activity. This may explain why many photosensitive epilepsy patients have cited fluorescent lights and other screen-related devices as prime triggers for seizures.
Intensity, brightness and contrast
Bright, sudden lights have a greater effect on the brain than softer, gentler ones. Strobe lights, camera flashes, and movie theaters thus carry the risk of a potential seizure. The light-to-dark ratio or contrast of a light source may also play a role in causing or triggering a seizure. This juxtaposition of intensely bright light followed by a sharp decrease in brightness (or vice versa) can cause the brain to become overstimulated.

Visual patterns
Although the intensity and speed of a light source are definite factors, we should also consider the pattern present within the lighting. Striped patterns—especially with high visual contrast and uniformity—have proven to be particularly dangerous for a photosensitive brain. Some researchers have even suggested that static images with these patterns can bring on a seizure, perhaps in as many as 30% of photosensitive epilepsy patients.
The risk may be even higher if the patterns have a moving component, such as outwardly-expanding circles, scrolling black-and-white stripes, wavy or zig-zag lines, or even pulsing checkerboard patterns.
Color or wavelengths of light
Certain colors of light have been identified as a possible culprit in provoking seizure activity in photosensitive patients. If a person also has migraine or other light-sensitive comorbidities, specific wavelengths of blue-green light can further aggravate these conditions—causing headaches, migraine attacks, seizures, or generalized light sensitivity as well.
Red light may be the most concerning if you are photosensitive because it can activate specific epileptic responses in the brain. Patterns or lighting that changes color to or from red also carries a possible threat for those prone to photosensitive seizures.
Distance
Although certain light sources may not be triggering in isolation, they may become risky if viewed at a close distance. For some with photosensitivity, something as simple as sitting too close to the TV may cause a seizure. Devices with LED/LCD screens such as smartphones, tablets, and computers also pose an increased risk; viewing them too closely overstimulates the eyes and brain.
Long-Term Impact of Photosensitive Epilepsy
As mentioned, photosensitive epilepsy seems to originate most often in childhood. While it can progress into adulthood and be passed down through genetics, there is encouraging news that perhaps as much as 50% of people with photosensitive seizures in their youth do not experience them later in life.
Even if you do continue to have these symptoms, there are ways to reduce the impact and threat of light-triggered episodes. And with extra caution and preparation, you can experience all the joys and activities of a normal life.
Photosensitive Epilepsy Management Tips
The most important step for managing photosensitive epilepsy is to be properly diagnosed. This may require a consultation by a neurologist as well as undergoing commonplace tests for epileptic patients—such as an Electroencephalogram (EEG), which records electrical activity in the brain under certain conditions (including its responses to light). We recommend working with your doctor to help figure out an effective game plan to manage your light-induced seizures.
If you have already been diagnosed, there are many ways to manage triggers related to photosensitive epilepsy:
- Changing computer and display screen settings for better comfort, e.g. avoiding high-contrast or striped graphics, activating motion-reduction settings, and disabling autoplay features
- Closing window blinds and covering up other contrasting light or visual patterns
- Opting for natural or warm lighting to avoid fluorescents
- Fixing any broken, flickering, or malfunctioning light (fluorescent or otherwise)
- Taking frequent breaks to rest your eyes
- Wearing polarized sunglasses for outdoor activities to reduce sharp glare (pro tip: TheraSpecs offers great specialty-tinted sunglasses for enhanced protection)
- If confronted with a trigger, completely covering up one eye and avoiding direct exposure
Photosensitive epilepsy glasses

In addition to the above recommendations, TheraSpecs offers a range of lenses that may help manage your photosensitivity to flashing lights and other aggravating light sources. In particular, TheraSpecs Z-Blue™ lenses (in max strength) filter most strongly in the red spectrum to provide the best protection against the brain responses associated with photosensitive epilepsy. This makes them perfect for concerts, movies, and other activities where flashing or intense lighting is common.
TheraSpecs also offers its FL-41 line of lenses, specifically for the harmful blue light from fluorescents and screens, which may also play a role in photosensitivity. Customers have been using our FL-41 lenses since 2012 to help manage their sensitivity to artificial and natural light, including flashing and strobing light patterns.
TheraSpecs can be further customized to meet your light sensitivity needs, with a variety of lens strengths and the ability to order prescription or reader lenses. Plus, we have a 60 day return policy covering most of our styles, so you can try them risk free!
References:
Panayiotopoulos CP. The Epilepsies: Seizures, Syndromes and Management. Oxfordshire (UK): Bladon Medical Publishing; 2005. Chapter 13, Reflex Seizures and Reflex Epilepsies.
Fisher RS, Harding G, Erba G, Barkley GL, Wilkins A; Epilepsy Foundation of America Working Group. Photic- and pattern-induced seizures: a review for the Epilepsy Foundation of America Working Group. Epilepsia. 2005 Sep;46(9):1426-41.
Hermes D, Kasteleijn-Nolst Trenite D.G.A, Winawer J. Gamma oscillations and photosensitive epilepsy. Current Biology. 2017; 27(9); doi: 10.1016/j.cub.2017.03.076.
Appleton R, Beirne M, Acomb B. Photosensitivity in juvenile myoclonic epilepsy. Seizure. 2000 Mar;9(2):108-11.
Harding, G., Wilkins, A. J., Erba, G., Barkley, G. L. and Fisher, R. S. (2005), Photic- and Pattern-induced Seizures: Expert Consensus of the Epilepsy Foundation of America Working Group. Epilepsia, 46: 1423–1425. doi:10.1111/j.1528-1167.2005.31305.x
Myers C, Mefford H. Advancing epilepsy genetics in the genomic era. Genome Med 2015; 7(1): 91.
Quirk JA1, Fish DR, Smith SJ, Sander JW, Shorvon SD, Allen PJ. Treatment of photosensitive epilepsy using coloured glasses. Seizure. 1999 Dec;8(8):444-9.
Kasteleijn-Nolst Trenité DG, Verrotti A, Di Fonzo A, et al. Headache, epilepsy and photosensitivity: how are they connected?. J Headache Pain. 2010;11(6):469-476. doi:10.1007/s10194-010-0229-9
Takahashi Y, Fujiwara T, Yagi K, Seino M. Wavelength dependence of photoparoxysmal responses in photosensitive patients with epilepsy. Epilepsia. 1999;40 Suppl 4:23-27. doi:10.1111/j.1528-1157.1999.tb00902.x
Kasteleijn-Nolst Trenité D, Acharya J, Baumer FM, et al. Frequently asked questions and answers on Visually-Provoked (Photosensitive) epilepsy. Epilepsy Behav Rep. 2025;30:100753. Published 2025 Feb 10. doi:10.1016/j.ebr.2025.100753
Last updated 28th July 2025

TheraSpecs® Glasses for Light Sensitivity
Find the glasses that fit your needs and lifestyle, and stay protected from screens, fluorescents, unwanted blue light, sunlight, flashing lights, and more.
Shop Now





