Fibromyalgia and Headache Disorders
Research has consistently shown a link between fibromyalgia and chronic headache disorders such as migraine and tension-type headache. The comorbid nature of these conditions can yield significant negative consequences, both physically and emotionally, for patients. We take a closer look at the experiences associated with the co-occurrence of these afflictions. Although it can seem grim on the surface, we also provide specific tips to better manage them and improve your outcomes.
How many people with fibromyalgia suffer from chronic headaches?
Among those who have been diagnosed with fibromyalgia, chronic headaches are one of the most common symptoms or comorbidities after generalized pain and fatigue. These ‘headaches’ can actually be diagnosed in many forms: transformed or chronic migraine (with or without aura), chronic tension-type headache, and cluster headache, to name a few. Although the statistics vary, researchers have suggested that a chronic headache comorbidity may exist in as many as 76% of fibromyalgia patients. Migraine tends to be the most common of these headache disorders, with separate studies showing that more than half had probable migraine.1-2
What is the physical impact of fibromyalgia and headache comorbidities?
Unfortunately, there are unique challenges if you have been diagnosed with both fibromyalgia and a primary headache disorder—especially chronic or transformed migraine. Patients may tend to experience a higher number of pain flares (approximately 20 per month) and were recorded as averaging 19 migraine attacks per month. For context, 15 migraine days per month fulfills the diagnostic criteria for chronicity. In addition, chronic migraine appears to have a direct influence on fibromyalgia flares, with 87% occurring within 12 hours of a migraine attack.3 This may mean that migraine acts as an independent ‘trigger’ for fibromyalgia. Although general pain levels are comparable, one small study did show worsening headache severity when both chronic migraine and fibromyalgia were present.4
In addition, each headache subtype can manifest with their own unique symptoms. Those with migraine may endure what is known as an aura or group of pre-attack symptoms, such as visual floaters or nausea. Similarly, head pain also varies: some experience stabbing headaches nearer the eye (cluster headaches), others have it localized to one side of the head and describe it as a dull throbbing (migraine), and even some do not have any cranial pain at all (migraine aura without headache). Even more complicated is that the physical symptoms are different for each person as well as from attack to attack.
Although the physiological effects are variable, research has shown that higher levels of pericranial tenderness in the muscles around the skull was reported by patients with both disorders. In a more recent study, chronic migraine patients were more likely to experience photophobia—or painful sensitivity to light—if they also had fibromyalgia.5-6 Our survey of light-sensitive individuals found similar results, specifically:
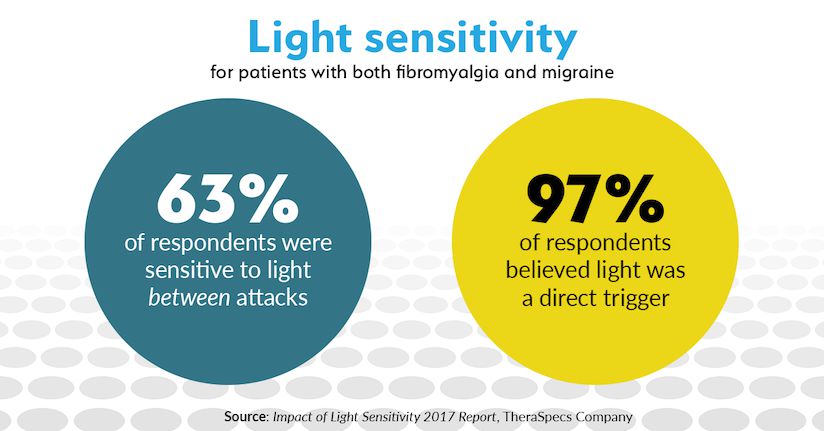
- Fibromyalgia was a greater predictor of light sensitivity and photophobia between attacks or flares (such as in pain-free periods) for migraineurs and chronic headache patients.
- 97 percent of respondents with both conditions reported that light was a trigger for pain and other symptoms. This was higher when compared with those who only had migraine or some other headache disorder.
Similarly, sensitivity to sound (known as phonophobia) was a common feature of both conditions.
Why do headache and migraine disorders worsen fibromyalgia symptoms?
Researchers also showed that there was a decreased threshold for pain at various sites on the body, including tissue, skin and muscle locations. While this is not surprising for either condition due to the high prevalence of sensory sensitivities, the tolerance for pain was significantly lower among those diagnosed with chronic migraine and comorbid fibromyalgia. This suggests that the two conditions may share similar pathophysiologies—or processes that contribute to the onset of symptoms. It is believed that hypersensitivity of the central nervous system characterizes chronic migraine and fibromyalgia and may thus be even more pronounced when occurring together. Another interesting theory has linked sleep disruption (a common side effect of fibromyalgia) with impaired responses to pain; in effect, patients are not able to ‘distract’ themselves from the physical pain when they are overly tired or fatigued.7
How does the diagnosis of both conditions affect quality of life?
If you already have chronic headaches associated with fibromyalgia, you are likely to notice a severe impact on your daily life. 84 percent have previously acknowledged that it has taken a significant toll on their everyday activities and productivity. They also had lower quality of life scores and higher levels of mental distress.8 Anxiety, depression and insomnia—independently associated with migraine and fibromyalgia—have also been observed at greater levels when they are both present.
Furthermore, the added complication of light sensitivity can worsen personal and professional outcomes. Our own analysis showed that sensitivity to light associated with these conditions significantly restricts work obligations, relationships with family members and friends, as well as the ability to go into department and grocery stores. With a high percentage of migraine and fibromyalgia patients also having photophobia, this impact can unfortunately compound the problem.
How can you treat fibromyalgia and related headaches or migraines?
Here is the big question, and it is not an easy one to answer. Doctors and specialists are still faced with finding ways to help manage the flares and attacks associated with these chronic conditions. At minimum, there are a few recommendations you can follow:
- Diagnose first. Overlapping physical symptoms can make it easy to overlook either of these disorders during the diagnosis phase. Amazingly, it may take up to five years to receive an accurate fibromyalgia diagnosis; and migraine (as well as its sub-types) are similarly under- or misdiagnosed. These new studies are incredibly valuable for practitioners and patients because they help narrow down the unique complications and side effects. Your doctor will likely utilize the International Classification of Headache Disorders (ICHD-3) resource and 2010 American College of Rheumatology Preliminary Fibromyalgia Diagnostic Criteria to evaluate patients. Make sure you document your symptoms thoroughly and have an open and honest dialogue with your physician.
- Focus on the headaches and migraines. Experts recommend concentrating treatment efforts on the comorbid conditions—in this case chronic headache or migraine. By getting these attacks and symptoms under better control, it can help isolate the fibromyalgia symptoms and allow for more targeted treatment on those issues. Additionally, medicinal prevention has previously helped reduce the total number of fibromyalgia flares; it also reduces the reliance on rescue medications and helps improve levels of pain tolerance.3
- Be cautious of prescription medications. This is an important one. In addition to the possibility of developing a new type of headache problem (known as medication overuse headache), prescription medications may compete with or complicate symptoms of the respective afflictions. The last thing a patient wants is to feel better with their chronic pain issues only to worsen their migraine attacks, and vice versa. For instance, milnacipran is FDA-approved to treat fibromyalgia but also lists headache as a frequent side effect. Ultimately, work with your doctor to find the right mix of medications.
- Address the emotional symptoms. It is natural to want to treat the pain of either of these conditions, and that should certainly be the primary focus for physicians. However, the impact of psychological symptoms (e.g. anxiety or depression) can be equally damaging. Psychotherapy is one option that can be helpful in managing these emotional challenges. In addition, finding ways to manage external stimuli—such as workplace accommodations related to lighting—can allow patients to maintain relative normal functioning and minimize productivity loss.
References:
1 Marcus DA, Bernstein C, Rudy TE. Fibromyalgia and headache: an epidemiological study supporting migraine as part of the fibromyalgia syndrome. Clin Rheumatol. 2005 Nov;24(6):595-601. Epub 2005 May 18.
2 Vij B, Whipple MO, Tepper SJ, Mohabbat AB, Stillman M, Vincent A. Frequency of Migraine Headaches in Patients With Fibromyalgia. Headache. 2015 Jun;55(6):860-5. doi: 10.1111/head.12590. Epub 2015 May 21.
3 Giamberardino MA, Affaitati G, Martelletti P, et al. Impact of migraine on fibromyalgia symptoms. The Journal of Headache and Pain. 2016;17:28. doi:10.1186/s10194-016-0619-8.
4 Peres MF, Young WB, Kaup AO, Zukerman E, Silberstein SD. Fibromyalgia is common in patients with transformed migraine. Neurology. 2001 Oct 9;57(7):1326-8.
5 De Tommaso M, Federici A, Serpino C, et al. Clinical features of headache patients with fibromyalgia comorbidity. The Journal of Headache and Pain. 2011;12(6):629-638. doi:10.1007/s10194-011-0377-6.
6 Cho, S.-J., Sohn, J.-H., Bae, J. S. and Chu, M. K. (2017), Fibromyalgia Among Patients With Chronic Migraine and Chronic Tension-Type Headache: A Multicenter Prospective Cross-Sectional Study. Headache: The Journal of Head and Face Pain. doi:10.1111/head.13191.
7 Campbell CM, Bounds SC, Simango MB, et al. Self-reported sleep duration associated with distraction analgesia, hyperemia, and secondary hyperalgesia in the heat-capsaicin nociceptive model. European journal of pain (London, England). 2011;15(6):561-567. doi:10.1016/j.ejpain.2010.11.014.
8 Ifergane G, Buskila D, Simiseshvely N, Zeev K, Cohen H. Prevalence of fibromyalgia syndrome in migraine patients. Cephalalgia. 2006 Apr;26(4):451-6.
TheraSpecs Glasses for Light Management
Try our light-filtering glasses and stay protected against harsh light from screens, fluorescents, LEDs, unwanted blue light, bright sunlight, flashing lights, and more.